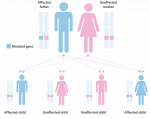
Hereditary angioedema (HAE) is a rare, serious, potentially life-threatening genetic disorder occurring in 1 in 50,000 to 1 in 150,000 people worldwide. In Europe, approximately 10,000 people are affected.1
People with hereditary angioedema (HAE) are unable to make enough of the functional blood protein, C1-esterase inhibitor (C1-INH). Lack of this inhibitor results in overproduction of an inflammatory substance called bradykinin, which causes leakage of fluid from blood vessels and build-up of excessive fluid, which is the cause of localised swelling.2,3
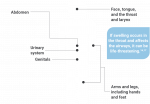
HAE causes repeated episodes of spontaneous angioedema – or swelling – that can occur at any time and in almost any part of the body but more predominantly in the hands, feet, face, airway (throat) and internal organs. Most people experience their first episode in childhood or adolescence. HAE is not an allergy or allergic reaction.5
HAE symptoms can start to occur at a very early age, but there are also examples of this occurring later in life. As incidents of suffocation due to throat swelling can occur within families with HAE, making a timely diagnosis is extra important.4
Typical symptoms that patients can look out for include:24,25
- Repeated episodes of abdominal (belly) swelling and swelling without itching
- Episodic attacks, with intervals between periods of swelling
- Onset of attacks in childhood or early adulthood, worsening around the time of puberty
- Episodes lasting 2-5 days in duration
- Family history of HAE
- Attacks not responding to corticosteroids or histamines
The diagnosis of HAE is made by a thorough clinical evaluation, a detailed patient history, and blood tests that test levels of the protein called C4 antigen.26 Other protein levels such as C1 and C2 can also be tested for. Ultrasound, CT scans, and X-rays may be used to demonstrate swelling.27
In Europe, expert centres have sufficient specialised, comprehensive care to make a reliable diagnosis.20 Diagnosis is obtained by laboratory tests performed on a blood sample. The blood of HAE patients shows a decreased concentration of C1-inhibitor and/or reduced activity of C1 inhibitor. The concentration of C4 antigen levels is also usually reduced in people with HAE.26